If you're reading this blog, you are already taking the steps you need to achieve intestinal (gut) health by cutting out grains and processed foods. Sadly, many people aren't aware of the brain:gut connection or that an unhealthy gut can adversely affect other areas of health. So I’ve asked my Naturopath, Dr. Melody Wong to guest post regarding gut health today. When I was in one of my worst flares, Dr. Wong helped me immensely by identifying trigger foods for me and placing me on a strict protocol of gut healing supplements and things to balance out my intestinal flora. Please welcome Dr. Wong to the blog today and feel free to leave any questions you have as she will be doing one more guest post as a Q&A. If you missed her introduction to Naturopathy last time, you can find it here.
Here are a few types of patients I commonly see in my practice. Do you identify with any one of them? If so, which one sounds like you?
Patient A: Frequent colds and flus : As a child – colds or ear infections came on one after another, causing many missed school days. As an adult- frequent colds turn into sinus infections leading to numerous antibiotic intakes
Patient B: Over worked, fatigue and exhausted : Career driven. Has long working hours. Doesn’t have time to cook. Eats out daily. Doesn't eat on time nor eats well. Possibility of having type A personality; a perfectionist who is frequently overly anxious and stressed out
Patient C: Food and environmental allergies : Has seasonal hayfever symptoms such as itchy eyes, nose, throat, or red watery puffy eyes. Reactive to common food items such as dairy and wheat. Symptoms can include indigestion after eating, abdominal pain, irregular bowel movements, etc.
Patient D: Difficult to concentrate and too tired to get through the day : Craves carbohydrates. Experiences Mind fog, fatigue, headaches, itchy rashes/eczema.
Patient E: Nervous Stomach : Colicky baby can’t seem to keep milk down and grows up looking pale with dark circles under the eyes. Any food intake doesn’t quite agree with the stomach. Irregular bowel movements. Never feels satiated nor has the appetite
What do all of these patients have in common? Whether these patients get ill frequently, are not taking care of themselves, have a history of all kinds of allergies, unresolved eczema, or stomach issues: most will end up having some kind of gastrointestinal (GI) conditions. All of which may include symptoms such as bloating, flatulence, belching, stomach aches, heartburn, indigestion, diarrhea, constipation, etc. Now does this start to sound more familiar? Is this happening to you? If so, you may now wonder how symptoms from the immune, nervous, endocrine, respiratory, and skin (integumentary) systems, lead back to the digestive GI system. Or perhaps does it start from the gut?
It’s really hard to say which came first. But nonetheless, healing and treating the GI is my primary focus in many of these cases. The GI tract makes up about 60-70% of the immune system. Once the immune system is compromised, it starts a chain of reactions. Initially, the nervous and endocrine systems will be overworked producing too much cortisol (an adrenal hormone), and later will produce too little. Neurotransmitters (excitatory and inhibitory chemicals) become imbalanced and indirectly cause a nervous stomach. Under stress, the GI system can become inflamed causing leaky gut, indigestion, and malabsorption of nutrients. Since histamine is stored and released in the gut, over production of histamine can cause inflammation and allergy symptoms in the digestive, respiratory and the skin systems. With all of these overlapping symptoms, patients frequently will have more than one GI condition. Here is a list of common GI conditions and symptoms I see in my practice.
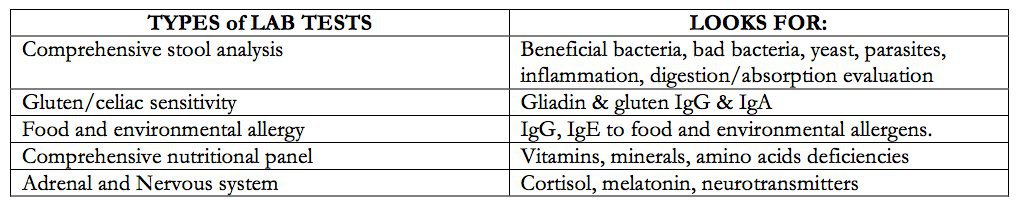
Besides listening to the patients for signs and symptoms, there are specific GI tests to differentiate between the types of GI conditions. Gastroenterologists would perform endoscopy and or colonoscopy to diagnose a patient for ulcers, IBS, IBD, or celiac disease, etc. Furthermore, the following lab tests are commonly done in a Naturopathic practice to provide possible causes and guidance to the appropriate treatments.
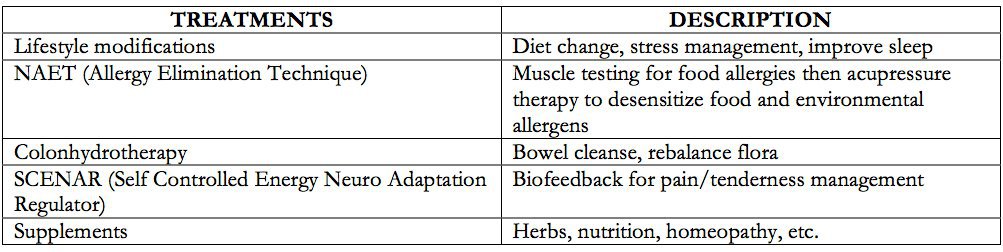
Conventional medicine typically will use pharmaceutical medications to manage the GI conditions some of which are antacid or H2 blockers for acid reflux or immunosuppressant for IBD. Naturopathic treatments that I would usually recommend, but not limited to, are the following:
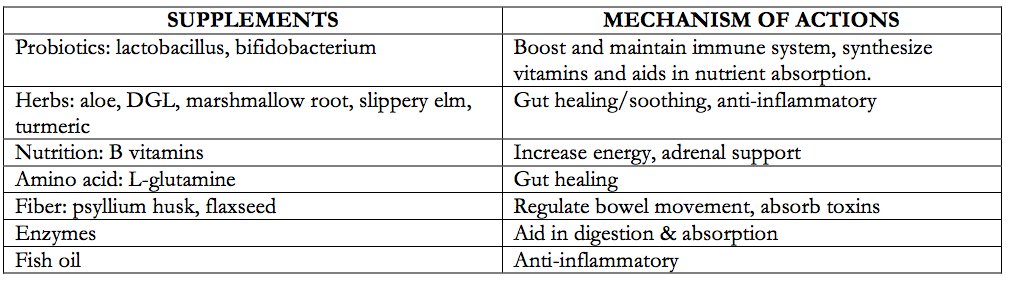
There are a plethora of supplements available for GI support, but I have put together a list of the most common ones I use for my patients.
This is plenty of information to digest and absorb in one sitting. I hope breaking it down in a chart format will give you a clearer picture. Ultimately for the best outcome, you need to find, treat, and heal the underlying cause of your symptoms. It is important to not self diagnose and treat. The Internet is a wealth of information, however, too much information may be confusing or even conflicting. I highly recommend seeking professional care from a licensed practitioner where you can be diagnosed and treated appropriately. I will be coming back as a guest one more time to answer your questions in a Q&A format, so please feel free to leave them below in the comments section.
About Dr. Wong
 Upon graduating from the renowned Naturopathic Medical School, Bastyr University, I returned to California and have been in practice for ten years. I believe the body has an innate ability to heal itself with the proper natural guidance. Most common conditions I treat in my practice are food and environmental allergies, gastrointestinal symptoms, fatigue, hormonal imbalances, and asthma/ eczema in pediatrics. Please refer to my website, www.banmc.com, for more information.
Upon graduating from the renowned Naturopathic Medical School, Bastyr University, I returned to California and have been in practice for ten years. I believe the body has an innate ability to heal itself with the proper natural guidance. Most common conditions I treat in my practice are food and environmental allergies, gastrointestinal symptoms, fatigue, hormonal imbalances, and asthma/ eczema in pediatrics. Please refer to my website, www.banmc.com, for more information.

Kim Owens
I’m all 5 patient types!!! Seriously! As a kid I was always sick and on antibiotics and steroids, took birth control pills, etc. I’m very much a Type A personality. I’m always tired, but can’t stay asleep at night in order to get a good night’s sleep. I’ve been diagnosed with Crohn’s disease, adrenal fatigue, and hypothyroidism. I’ve made so many changes to my diet and lifestyle, but I know there are still more needed. I guess my question is…how do you treat the patient who is all 5?!!!
Jessica L.
You just described me as well! I have also been diagnosed with Crohn’s and Hypothyroidism. Im anxious to see what her response is. I feel like im doing alot of what was mentioned…SCD diet, digestive enzymes, probiotics, fish oil but i know there is alot more to learn and a long way to go. Looking for some direction?!?!
Lori
I have a question regarding eczema. Both of my boys have Celiac Disease and horrible eczema to the point of bleeding and scarring their legs. We tried eliminating several things from their diets, but it never fully went away. We eliminated grains, yeast and milk for almost a year (they obviously don’t eat gluten). It seems to go away in the summer, though. Could some eczema JUST be weather related since the air is so dry in the winter? With colder weather upon us it is coming back and I’m wondering if I need to do an elimination diet again and if I am missing something. I will say, though, upon reintroducing milk to my youngest he had a HUGE growth spurt. We eat very healthy meals (not processed, lot of fruits and veggies…) and they do take a daily, vitamin.
Catie
Lori:
My 6 year old son has eczema issues too. When we tackled his diet, allergies, & skincare products, the eczema all but went away…only to return this year when the weather changed. His diet is still the same, and we haven’t used any new products, so I’m blaming it on the weather. I got a hold of some raw, unrefined shea butter (which is really thick) and I’ve been slathering it on him morning & night for over a week now. It’s improved a lot, and he isn’t getting any new spots. He’s not itching as much, and the scabby areas have healed. Maybe this will work for your boys? I’m also giving him fish oil to ease any internal inflammation.
Lori
Thanks for the reply. I have used Pure Organic Shea butter for a few years now, with no change. It will get better right away, but then goes back to the same condition as it was before. We only use organic shea butter and organic soaps. Again, when we switched it got better, but not for long. My kids legs are getting scarred and I refuse to put the dangerous hydrocortizone creams that aren’t a cure, but just a cover up. Have you noticed any change with the fish oil? I haven’t tried that.
Susanne
I know this is an older comment, but in my son’s case the eczema on his legs is caused by a mild dust mite allergy. In summer he is clear most of the time, but as soon as the dust mite season starts he will get more and more eczema. If I keep the dust mites at bay his skin will clear up again. He doesn’t have any problems with his airways, btw.
Adrienne
Great post! I am wondering a few things:
1. What do you think about NAET? I have heard a lot of interesting things about it, ranging from “It is amazing” to “It is no different from placebo and has no scientific evidence backing it up.”
2. Do you have a digestive enzyme that you recommend?
Thanks again!
Lisa
What do you think about the use of chiropractic to help heal digestive problems? I’ve heard that if you have a misalignment your body will not be able to heal properly as the message from the brain to heal can not properly get communicated to the rest of the body. As chiropractic care can be very costly, I’m wondering if this is true and warranted. Thanks for your help!
Mary Lethbridge
I was diagnosed with H-pylori about two years ago and the prescribed antibiotic seemed to work for about six months, but all the symptoms came back. I reluctantly tried another round of the antibiotics along with a probiotic in hopes to keep what good bacteria I had left, if any. Unfortunately, after a breath test 6 months later, I am still infected with H pylori. I would love to know if there is a natural way of ridding my body from this thing. I have started drinking kombucha, drinking beet kvass and eating fermented sauerkraut which seems to help a little, but I still experience bloating, flatulence and pain sometimes. Any advice you may kindly offer would be very much appreciated. I do believe it all starts in the gut as well, and I desperately want good gut health back. Do you know of any natural remedies to rid my body of this h pylori? Thank you.
Randa
Mary, this is a bit late but wanted to chime in. I am not a medical professional or expert, but have read that mastic gum (from Greece and that general area) can be helpful in cases of H-pylori. Perhaps research this?
Hope it helps!
Rebecca Prange
Hello Melody,
Thanks for guest posting about such an important human health issue. I’ve been healing a seriously damaged metabolism for almost 20 years now and am still finding new information helpful. My question for you is about Alfalfa. I was drinking alfalfa tea for an overall health benefit, then read that it contains starch that may not be good for my gut. What is your opinion/experience on/with alfalfa?
Lynn Liles
Your posts have been so informative. If I lived on the west coast, I would definitely come see you. I’ve been seeing an acupuncturist in my area. She has been terrific, but sadly, because of her own health issues, she really doesn’t have the time to give to her patients. I’ve been having GI problems for most of my adult life. I know I’m allergic to dairy, buckwheat, amaranth, clams and mussels. Can’t really get my acupuncturist to get around to any more testing to see what’s really going on. If I eat wheat, it’s a nightmare. I get allergy shots and am on a multitude off meds for my allergies and stomach. I won’t continue, but I’ve printed your list of supplements and am going to combine that with a Paleo diet to see if I can get any relief. Right now, I’m just suffering. Thank you for your information.
Sincerely…Lynn
Jeff Lembke
Hi Melody, I have many of the issues you mention here, with the added displeasure of severe “benign” heart palpitations (PVC’s) that come on in tandem with these issues. It is extremely distressing, and the only relief I’ve found is to take DGL, anH2 blocker, AND a PPI (prilosec) daily. Even then there are stretches where this doesn’t work. My gut is nearly always in a bizarre turmoil, and I frequently am woken up at about 4:30 or 5:00 AM with diarrhea, severe palpitations, and resulting anxiety. In addition, my lymph nodes and thyroid have been swollen for months if not years, and my platelet count is low. My doctor, also a graduate of Bastyr, says all test show there is nothing serious (cancers etc. thryoid working fine) going on and I recently tested negative for h.pylori. I have a very limited diet now, but that doesn’t seem to be solving the problem. Do you have any ideas for what someone in that position should do next? My fear is that there is something destructive going on in my bowel, and nobody and think of how to diagnose it.
Thanks for your great input on this website.
Ann
Jeff, you sound just like me! There is a very strong connection between the gut and the brain, and it sounds like you have already realized this. I was hospitalized several times early this year with what I thought were heart “issues” only to find out my heart is healthy and strong. What I was experiencing were panic attacks.
After being diagnosed with anxiety and a “panic disorder” I was put on an antidepressant and given Atavan for the anxiety. Yes, I have benefitted from both, however there were still just too many times that the meds gave me NO relief. I couldn’t stop thinking that there was a physical issue behind a lot of the anxiety.
After having a few weeks this year where I was nearly incapacitated with the physical symptoms of being in such a high-alert state for days at a time, I finally started seeking help from an acupuncturist and herbalist. She prescribed two herbal blends, one for my gut and one for the mental/emotional aspect. I started taking the “GI Harmony” for my gut right away and was feeling quite a lot of relief within a couple of days. The other blend is helping as well, but I give most of the credit to the herbs for the gut. The blends are from Evergreen Herbs, and they are prescription items. The gut formula is called “GI Harmony” and the formula for the mental and emotional aspects was called “Calm ES”. They are made from recipes for Chinese herbal remedies, and I am having very good luck with them.
You know that term “butterflies in the stomach”? Mine were pterodactyls! It’s been such a RELIEF not to be walking around hating my life every day because I constantly had the feeling that the worst thing ever was about to happen.
Some good books on the gut-brain connection are “Gut and Psychosis Syndrome” by Dr. Natasha Campbell McBride, “The Second Brain” by Michael D. Gershon, and “The Anti-Anxiety Food Solution” by Trudy Scott, C.N.
Good luck on your quest for health!
Inna
Hello Melody!
I really enjoyed your post!
Can you recommend any doctors in New York City?
I would love to visit a naturapath for all of the above reasons, however I don’t know how to find a trusted one.
Thank you.
Dr. Melody Wong
Hello Inna,
I recommend Dr. Donielle Wilson.
Here’s her website:
https://www.doctordoni.com/welcome.html
Best Regards,
Dr. Melody Wong
Sylvia
Thank you for all the helpful information. Could you please tell us when it is best to take probiotics – before or after a meal and also how long before or after a meal. How many times a day? Do you have any you recommend? What do you think of VSL#3?
Dianne G
I have been loosely following a gluten-free diet for about 6 years, but started to develop ibs symptoms a year ago. I googled it and found a program based on proper food combining ((not mixing starches with proteins, with the exception of beans and nuts, which can be combined with either)). Enzymes and probiotics are also recommended.. I have had terrific success! I’ve shared this info with friends and family suffering GI problems, and it’s helped them as well. This past month I have cut back, then eliminated all grains, even gluten-free grains. I make “bread’ using almond flour, almond butter, and/or coconut flour instead of flours from grains. these are Paleo bread recipes. Pain and inflammation in my legs and knees have disappeared. I can walk up stairs, or get down on the floor pain-free, (and without worrying if would be able to get back up!). I’m totally sold on this new way of eating. Does your practice ever include food-combining?
Donna Scarcella
Hello, I live in the Tampa Bay area and am looking for a Dr. here like Dr. Wong.
Do you have any referrals?
Thank you,
Donna Scarcella
Tracy W
Hi, Melody!
I live in the Issaquah/Seattle area and was wondering if you could recommend a great naturopath in my area. It’s time to start healing my body and would love to use a highly recommended naturopath.
Thank you very much!
Tracy
Dr. Melody Wong
Hello Tracy,
I recommend Dr. Phoebe Yin.
She’s a professor at Bastyr University and also has her private practice via Bastyr Center for Natural Health. Feel free to mention me.
Best Regards,
Dr. Melody Wong
Carol
Thank you for this guest post! I love hearing about how I can heal my gut. It’s so important!
amber
Great information, Danielle! Glad to read that I take nearly all those supplements. Makes me feel like I am doing something right! 🙂
Thanks for sharing Dr. Wong with us. She’s fantastic.
Hugs,
–Amber
Jessica
A very informative post! The charts were helpful. There are a lot of great questions posted that I would like to see answers to…and I do have my own.
I started having allergies for the first time at the age of 26, ten years ago. A year later I was diagnosed with asthma and could not smell or breathe through my nose. I had nasal polyps and they were removed surgically in 2006 and again in 2007. I just had my third surgery removing the polyps a couple weeks ago…..and already my DR says they are growing back. I just learned of good nutrition practices a few years ago, so yes, I ate the SAD for many years. I desperately want to smell and breathe, which means getting rid of the nasal polyps, besides get rid of the allergy problems. I take zyrtec and singulair every day, year round and have for the past 10 years. If I stop taking them, I start coughing all the time, runny, dripping nose constantly and my face/nose/throat itches like crazy. The only obvious digestion issue that I deal with would be constipation occasionally.
Any suggestions?
Kimberly
Goodness gracious! I am all five as well! Although, my problems have forced me to eat fairly well at least to the best of my abilities! My goodness.
MP
I loved your information about digestion. My main question would be how long do you take the various supplements such as L. Glutamine, Zinc etc. and also the enzymes? Also I have been taking the above and feel that it is helping but then that leads to constipation. How do you alleviate that issue when taking your vitamins and supplements? If I stop then I feel symptoms return.
Thank You
Kerry
Thanks Dr. Wong, My question is about healing crises. A few months back after years of gluten and dairy-free I went Paleo. About a month ago I added the AIP. I was feeling better than I have in a very long time, and then whammy. I’ve been told by my conventional doctor I’m probably having a relapse of MS, but I truly wonder if it isn’t a healing crisis. How do I tell the difference? How would you define a healing crisis?
kristin
Great post! My daughter, 6, has been battling ulcerative colitis for almost a year now. We practice SCD 95% of the time (it’s really hard for a 6 year old 100% of the time). It has been a two steps forward, one step back process so far. I was wondering if some of the supplements you recommend would not be suitable for a child. She takes a daily probiotic but I have been thinking of introducing L-glutamine and possibly aloe. Her bathroom visits are not normal right now since she ate two peices of Halloween candy but it is not out of control either. Can these supplements be introduced during a flare period or should her stools be somewhat normal. Thank you for all the information you can give.
Anne Allen
I dealt with yeast overgrowth for many years….have had no problems for the last 2. I avoid probiotics with FOS and any products with yeast. I”m curious from your experience if FOS can trigger yeast overgrowth?
thank you
Adrienne
Hello there. I am interested in everything that you wrote, but I can start with 3 questions, if that is OK:
1. Primarily at this point, I am curious about NAET. I have heard of many success stories, but I have also heard that the studies on show that it is no more successful than placebo. Can you speak to this?
And it appears from your post that you think it is highly important to do all of these tests (the ones that you recommended) in order to sort out what area needs to be targeted, correct? Do you see that once that is done you are able to help the majority of your patients to the point that they are “cured”?
Finally, I am assuming that “curing” does not permit the patient to go back to eating a poor diet, right? I am wondering why there are so many folks eating horribly but without the issues that those of us who deal with a plethora of issues have. Could you address that as well?
Thank you!
Heather
I would love to know what Comprehensive Nutritional Panel you test with. I am blessed to have learned and gone through a lot of what is mentioned in this post – however, one thing that I believe would be beneficial for me is a quality nutritional test – to see if I’m deficient in some very important nutrients! Thanks so much for sharing this wisdom with the readers!
Sue
Hi, I am presently being treated for Candida and Leaky gut due to many food allergies and everything else you describe. I’m frustrated because my 7 year old grand daughter has eczema and breaks out in the summer sun to the extent that she gets feverish, her eyes swell up and the itching is intolerable causing her to wear mega protective clothing even in the worst heat and often she just doesn’t want to go out and play. She also has very thick, black, sticky stools. To me this all screams of food allergies and a gut issue but my daughter doesn’t want to hear it. What’s your take?
SC
Can you please recommend a NP in the Fort Collins or Denver Colorado region? Thanks do much!
MJP
I am also following SCD Diet, and taking the supplements such as probiotics (SCD Legal) fish oil, L Glutamine (not sure how long to take this or do I take it daily?) and feeling pretty good. What is the next step since if I falter just a little off the SCD diet my symptoms return. Also have SIBO per my MD and maybe Candida. Not sure
what to do next. What is your advice? Also can you tell me a good Naturopathy doctor in Raleigh, NC.
Thank You
Gd
I would recommend Dr. Dishman in Raleigh, NC.
Julie Martin
Thank you for this informative post. I’m familiar with all the supplements you listed. Is there a brand you suggest, specifically for the l-glutamine, enzymes and fish oil? I know no two brands are made equally.
Thank you.
Andrea
Hi!
I’m hoping you can recommend a Naturopath in Boulder. There’s almost too many alternative dr’s to choose from.
Thanks!
Andrea
Harmony
Hi-I was hoping you could recommend a brand of probiotics.
Thank you
Amelia
Any recommendation for a Naturopathy Doctor in Kansas City?
Fam Hens
Dear Dr. Wong,
My husband has cronic fatigue. IT started after a bronchitis in 2014. In the beginning of 2015 (after finding out we were to have a baby) he couldn’t walk the stairs or stand to long On his feet . His wonderfull new job had to let HIM go , so HIM being our financial provider gave us a large set back. We’ve been true a whole check up at the hospital And just before the Arrival of our daughter they said on paper theres nothing wrong with him so he must have chronic fatigue….
Our house docter doesnt have clue …. by looking for help on the internet we are thinking About naturopathic. In dutch called orthomoleculair doctor i think…
So here for our question:
How would you treat a patiënt like this? Or what are the signs you know you are working with a Pro in the field. In the Netherlands Everyone can practise iT but there are Some who worked as docters before they practice naturopathic..
Naturpathic costs Will come out of OWN pocket so we really dont have the liberty to go to several before we find the one who can help us.
Of something comes to your mind about our situation we would like to here iT
Ps paleo is something we do.
Next to cronic fatigue he always had “Renaud” And in his 20’s was diagnosed with reflux .
Thank you for responding
Familie H. From the netherlands near the hague
Bridget Eichelberger Wintle
Any suggestions for a NP in Utah (Salt Lake City area). My son was diagnosed with Ulcerative colitis in 2015 at the age of 12 and hospitalized in 2016 after he lost 20+ lbs from an allergy to his medication. They put him on Remicade at that time and has an infusion every 8 weeks. I always ask his GI doctor if there is something different he needs to do with his diet and he says “no, don’t worry about it”. My son is 14 now and I just see a life of hard core meds and the huge medical costs that come with it. This article has got me thinking about the food connection again. He is a very picky eater and most of what he likes are proteins and carbs with a few choice veggies. I know it will be hard but I feel like he could be managing his symptoms with food more than meds.